We all complain about how fast summers seem to fly by. I can’t recommend it, but try having a potential cancer diagnosis, then waiting for your follow-up consult from the end of June to the end of August.
On March of 2018, I coughed up a bit of blood out of the blue. A life-long severe asthmatic, I reflexively checked in with my doc who ordered a CT just in case. No real concern, I run, eat healthy (well except for chicken wings), never smoked, etc. All-in-all pretty innocuous, no real urgency either.
At the end of June, just 3 days after finishing a half-marathon, I had the CT. Bing-bang-boom, the test was done, and I was on with my day.
Until 90 minutes later when my doctor’s office called to book an urgent appointment the next day. My guts sank.
I spent the next 24 hours agonizing over her quick response.
Upon arrival she was visibly upset and told me point blank the news wasn’t good and she was completely shocked by the result.
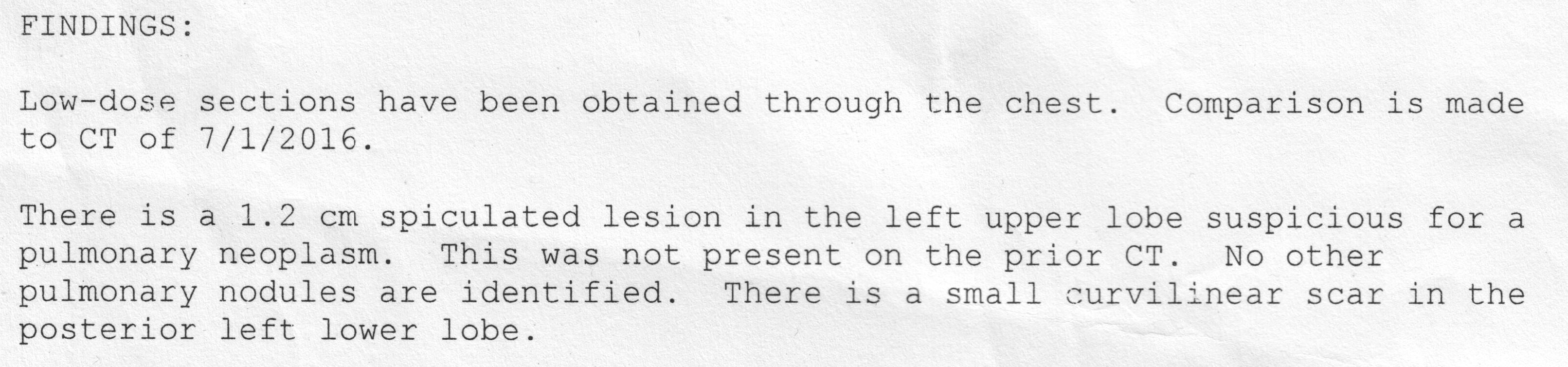
I had a 1.2 cm spiculated lesion in the upper lobe of my left lung, where there had been nothing a year-and-a-half earlier.
The real concern seemed to be the word “spiculated,” a word no clinician likes to see. It carries a certain connotation, loosely translated as, “hol-ey shit, you’re screwed!” Ninety percent of such lesions turn out to be malignant.
Reassured that the radiologist’s written report saw no other potential involvement, she felt it had been caught early. She got her staff right on setting me up for the next stages: confirmation and treatment—most likely surgery. Stoically, I held off telling anyone until I knew more to avoid worrying people unnecessarily, especially my wife and kids.
But this was just before the Canada Day long weekend, the unofficial start of summer, so nothing clinical would happen the next day. Or the next week. Clearly, I needed a better plan.
The day before my next GP appointment, I got my consultation booking with the surgeon—by regular mail. It was a summer-and-spirit-crushing two months away (with no idea when I would have a follow-up CT).
I called the surgeon’s office to see if I could get more information or speed up the process. Her assistant rotely informed me that the surgeon simply didn’t get cancellations and there was really nothing that could be done. So that was that.
Like a lot of severe asthmatics, I have many co-morbidities, chief among them a real honest-to-goodness diagnosed anxiety disorder. So, I finally and completely fell apart. And now HAD to tell my family and friends.
I shared the potential diagnosis with my wife, who used to work in cancer clinical trials. She, too, was unable to glean more. Likely the hardest thing I have ever had to do was tell my 19-year-old son and 12-year-old daughter that I could have lung cancer. I can tell you that any vestige of composure vaporized. Telling parents, family and friends occurred in a fugue-like numb fragility.
My summer was a torturous Groundhog Day-esque trip into depression, anxiety flares, and support seeking. Something I plan to write about—but later. Suffice to say that despite the final outcome with the lesion, I still suffer.
My follow-up CT was finally scheduled for two days before my surgical consult. But, in a perverted twist of deja vu, the day before the consult I got a call from my doctor’s office. To my surprise, it was my actual doctor, not one of her staff. She said, “Bill, are you sitting down?” As I had pulled over to take the call, I was indeed. I did not know what to expect, but she sounded elated.
“It’s gone.”
“I’m sorry,” I sputtered. “What’s gone?”
“The lesion.”
I sat in stunned silence. She continued, “I have only had this happen once before in my practice.” After an awkward exchange I got off the phone and just sat there. Then drove around aimlessly for a while. Finally, I made a few calls, but told everyone to wait until I had the surgical consult the next day before announcing it more broadly.
But. It. Was. GONE.
At my consult, I told the surgeon I already knew the second CT results. But I still wanted to understand what had happened. I wanted to see the two CT images. I wanted clarity. I wanted answers.
What I learned left me dumbfounded, speechless and seething.
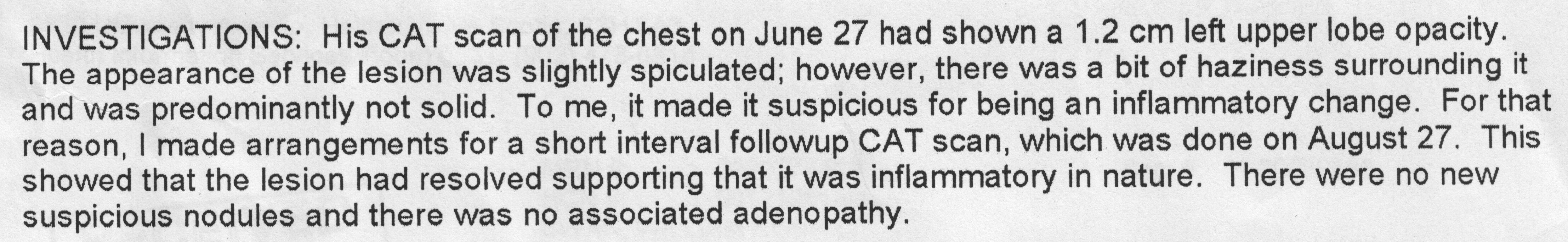
The diagnosis I had received wasn’t a consensus. In fact, the surgeon had reviewed the initial report and imagery a few days after the initial radiology report in June and felt that it didn’t actually show spiculation at all. To her it looked more “hazy,” and consequently much less worrisome. Probably just a mucous plug. As a result, the confirmation CT and consult had been set for the end of the summer to see if it was just something transient.
I sat enraged, bewildered and utterly paralyzed. Why wasn’t this information immediately passed on to myself or my doctor?
Within a week, a staff radiologist and a thoracic surgeon had come to opposite conclusions, yet no-one felt it important enough to inform either myself or my doctor.
Doing so would have changed my summer. Doing so would have kept me from dropping into a depression that I continue to grapple with.
And no-one thought it important enough to investigate—or even discuss—why there were different interpretations between two specialists.
The radiologist who initially reviewed the CT in the public system is also Medical Director of a local private medical imaging clinic. Is it possible that this split allegiance with the private sector affected the quality of the review of my CT in the public sector? Is this the first time this has happened with this radiologist? Has there been other similar incidences with this radiologist?
Most galling of all?
Fixing this would not involve any significant cost, no intensive study, no major change in administration. Fixing this is as simple as treating the patient with the most basic of consideration—respect. A simple letter or e-mail from the surgeon.
Let me be clear, I wasn’t clamouring to be healed immediately, nor was I looking for some high-cost miracle.
From the start of this mess, I just wanted information. Information that—as it turns out—was just sitting there. Tantalizingly close yet completely out of reach.
If we truly want to create “learning health systems,” the de rigueur term for health reform, something needs to change. But it won’t until our system truly comes to terms with what patient-centricity is and its crucial importance in all aspects of the health care system.
And let’s remember something. Something critical. If it weren’t for patients, a LOT of people would be out of work.
Bill Swan is a Nova Scotia activist who advocates for universal pharmacare. Check out his website Faces of Pharmacare, real stories from real Canadians about how the healthcare system fails them.
With a special thanks to our generous donors who make publication of the Nova Scotia Advocate possible.
Subscribe to the Nova Scotia Advocate weekly digest and never miss an article again.